
Healthcare Communication: The Detailed Guide for Clinics & Teams
Miscommunication is costly in any business.
A wrong marketing email might cost a sale.
But in healthcare communication, the stakes are higher. That error can delay treatment, contribute to patient harm or even lead to preventable deaths.
The numbers are sobering. Research shows that poor communication contributes to about 24% of patient safety incidents, including medication errors and near misses and is the sole cause in roughly 10% of cases.
CRICO Strategies also found that, out of 23,000 malpractice lawsuits reviewed between 2009 and 2013, communication failures resulted in 1,744 deaths and $1.7 billion in malpractice costs.
Healthcare communication isn't just about patient education or clinical handoffs..
It's also about how your marketing team engages the community, how leadership reports performance metrics to the board, how operations coordinates across multiple facilities and how your organization aligns thousands of employees around shared goals.
When any part of that system breaks down, the ripple effects are felt across the entire organization.
In this guide, I’ll walk you through everything you need to know about healthcare communication. I’ll discuss key challenges, proven frameworks, best practices backed by research, essential tools for your tech stack, real-world examples and templates and how AI can optimize your healthcare communications strategy.
Disclaimer: Visme is not a HIPAA-compliant platform and should not be used to store, process or transmit protected health information (PHI). Users are responsible for ensuring their use of Visme complies with applicable data privacy and security regulations.
Quick Reads
The Community Guide defines health communication as:
“The study and use of communication strategies to inform and influence individual and community decisions that enhance health.”
This definition captures the core purpose of health communication: helping people understand information, make better choices and take appropriate action to improve health.
In practice, health communication is how healthcare organizations turn medical and operational information into something people can actually understand, trust and act on. But it’s not limited to patient education or public health messaging. Healthcare communication includes every piece of information that moves inside or outside a healthcare organization:
Patient interactions. How you explain diagnoses, treatment options and care plans. How you educate patients on prevention. How you support them in making informed decisions about their health.
Internal coordination. How clinical teams hand off patients between shifts. How new protocols are rolled out. How staff are alerted to safety issues. How departments stay aligned across locations and roles.
Leadership reporting. How raw clinical and operational data is turned into dashboards that executives can use. How performance metrics are communicated. How trends, risks and opportunities are presented for decision-making.
External messaging. How you build trust in your community. How you attract and retain patients. How your organization is positioned. How sales teams communicate value to partners, payers and providers.
When health communication is effective, people across the healthcare system—patients, clinicians, leaders and partners—can clearly see what's happening, understand what it means and know what to do next.
Healthcare runs on information.
Every diagnosis, treatment decision, handoff and outcome depends on someone understanding something correctly and acting on it.
When that communication works, patients recover, teams coordinate seamlessly and organizations thrive.
But when it breaks down, the consequences can range from frustrating delays and duplicate work to medication errors, preventable readmissions, malpractice claims and patient deaths.
Here are a few reasons why effective healthcare communication matters at every level.
Poor communication is a leading cause of sentinel events and medical errors.
When patients don't understand their medication instructions or when prescribing information isn't clearly communicated across care teams, the results can be fatal. The Joint Commission found that communication failures were the root cause of over 70% of sentinel events in hospitals. These are events that result in death, permanent harm or severe temporary harm.
On the flipside, improving healthcare communication delivers concrete results. Studies show that when physicians communicate clearly and compassionately, patients have better adherence to treatment plans, experience less anxiety and report higher satisfaction.
I already mentioned earlier that communication failures contribute to malpractice costs. But the financial impact extends far beyond legal fees.
Preventable hospital readmissions cost Medicare approximately $17 billion per year, with many caused by inadequate discharge communication. When patients don't understand their care instructions, warning signs to watch for or follow-up requirements, they end up back in the emergency department. And that translates to avoidable strain on both the patient and the system.
Inefficient internal communication wastes significant staff time and resources. Research shows nurses spend up to 25% of their time searching for information, clarifying orders or tracking down providers. When protocols are unclear and communication handoff is poor, it causes redundant work, delayed care delivery and drains resources.
Communication quality is one of the strongest predictors of patient satisfaction scores, which directly impact hospital reimbursement under value-based care models. HCAHPS scores place more emphasis on communication metrics, and hospitals in the lowest-performing quartile can lose up to 2% of their Medicare reimbursements.
When patients feel heard, informed and respected, they're more likely to follow treatment plans, return for follow-up care and recommend your organization to others.
Poor communication also causes patient churn. According to the Glaucoma Research Foundation Patient Survey, 60% of patients switched providers because of communication-related issues. They left because they felt rushed, weren't listened to or didn't understand their care plan.
Regulatory bodies increasingly focus on communication standards.
For example, the Centers for Medicare & Medicaid Services (CMS) requires hospitals to meet specific communication benchmarks to avoid readmissions. The Joint Commission's accreditation standards include detailed communication requirements for handoffs, patient education and informed consent.
Failure to meet these standards results in penalties, failed inspections and potential loss of accreditation. But beyond compliance, effective communication protects organizations from litigation. Proper documentation, accurate informed consent processes and transparent patient communication reduce legal vulnerability and demonstrate standard of care.
Effective communication is the foundation of good decision-making in healthcare. Leaders at every level rely on accurate, timely information to allocate resources, manage staffing, evaluate performance and set priorities.
When communication is effective, data from clinical outcomes, patient feedback and financial performance are shared and understood in context. This allows leaders to act quickly and confidently instead of making decisions based on partial or conflicting information. And research shows that organizations with effective internal communication strategies are about 3.5 times more likely to outperform their peers in overall performance metrics, including decision-making and strategic alignment.
Healthcare organizations operate in a constant state of risk, where system outages, safety events or public health emergencies can happen at any time. In these moments, clear communication becomes the backbone of the response.
Studies on crisis communication show that having well-defined communication protocols enhances organizational resilience by improving coordination and reducing anxiety during interventions and other stressful events.
In healthcare specifically, strong crisis communication also helps ensure that patients, staff and external stakeholders receive consistent, accurate information when it matters most. Teams can coordinate faster, reduce confusion and prevent secondary errors during high-pressure situations.
Communication breakdowns in healthcare are not subtle. They’re pervasive and consequential.
So why is it so difficult to address these issues?
Because healthcare communication doesn’t fail for just one reason. It breaks down at multiple points between patients and providers, across care teams, inside complex systems and under constant time and compliance pressure.
For example, language and health literacy gaps alone are a big deal in the health sector. In the U.S., about 26 million people have limited English proficiency, which correlates with increased misunderstanding, misdiagnosis and barriers to care.
But that’s just one of the several issues.
Below are the key barriers that make effective healthcare communication difficult and worth tackling.
| Healthcare Communication Challenges | Explanation | How to Overcome Them |
|---|---|---|
| Medical Jargon | Clinicians use technical terms that most patients don’t understand, which leads to confusion about diagnoses, treatments and next steps. | Use plain-language explanations, visual aids and teach-back methods to confirm understanding. |
| Language Differences | Patients and providers may not share the same language or level of fluency, making it hard to explain symptoms or give instructions. | Provide professional interpreters, translated materials and multilingual digital tools. |
| Low Health Literacy | Many patients struggle to find, understand and apply health information, especially during stressful situations. | Simplify written and verbal instructions, use visuals and avoid unnecessary medical terms. |
| Cultural Differences | Beliefs and norms about health, illness and treatment vary across cultures, which can affect trust and engagement. | Train staff in cultural competence and ask patients about their preferences and beliefs. |
| Emotional Barriers | Fear, anxiety, pain and stress can prevent patients from processing or sharing important information. | Practice empathetic communication, allow time for questions and provide reassurance and support. |
| Disabilities & Accessibility Issues | Hearing, vision, speech or cognitive impairments can limit how patients receive or give information. | Use accessible formats such as large print, captions, assistive devices and clear, simple language. |
| Interdisciplinary Communication Gaps | Information doesn’t always flow smoothly between doctors, nurses, pharmacists and other care providers. | Use shared documentation systems, standardized handoff tools and regular team briefings. |
| Time Constraints | Short visits and heavy workloads reduce the opportunity for thorough communication. | Use structured checklists, pre-visit materials and follow-up messages to reinforce key points. |
| Technology Barriers | EHRs, portals and digital tools can distract from personal interaction or exclude patients without access. | Balance digital tools with face-to-face communication and provide training or alternative options. |
| Complexity of Health Information | Medical topics are detailed and constantly evolving, making them hard to explain clearly. | Break information into steps, use visuals and summaries and provide written take-home materials. |
Healthcare communication is built on five fundamental components that work together to ensure effective information exchange between healthcare providers, patients and communities.
The components I’ve shared below are backed by communication science and public health frameworks used globally.
And understanding them will help you deliver messages that lead to positive changes in knowledge, attitudes and practices.
Made with Visme Infographic Maker
The source is the originator of the message. In healthcare, the source can be an individual, a team or an organization such as a doctor, nurse, clinic, hospital or public health agency.
People are most likely to accept communication from sources they trust and consider reliable.
And credibility is established through several factors. A person's natural position in the family or community, such as being a household head, village chief or elder, can provide authority.
Personal qualities and actions also build trust. For example, a health worker who consistently helps people, even during nighttime emergencies, earns credibility through dedication.
Respect for qualifications and training further strengthens the source's authority. Additionally, when the source shares characteristics with the receiver—such as age, sex, education, religion or life experiences—the message often resonates more effectively.
The receiver or audience is the person or group for whom the communication is intended. Identifying and understanding your audience is the critical first step in planning any communication. You must ask: Who is your audience? Do you have primary and secondary audiences? What information do they need to take action?
Audiences typically exist in layers. For example, when Health Extension Practitioners teach about family planning, couples from the community form the primary audience—those who will directly use the information.
Grandparents and other family members become the secondary audience, as they influence family decisions.
The tertiary (third) audience includes other people in the wider community who may indirectly benefit from or be affected by the health message.
A message is the information being communicated. It can include facts, instructions, opinions, feelings, attitudes or calls to action.
In healthcare, messages are rarely just informational. They are designed to influence understanding, decisions and behavior.
To persuade people and drive action, you need to organize your content using different appeals. That’s primarily because not everyone responds the same way. What motivates one person may differ entirely from what motivates another.
For example, people with little or no formal education may respond to different appeals than those with higher levels of education. Children process messages differently from older adults.
To reach a diverse audience, healthcare communicators use various types of appeals:
A channel is the medium through which a message travels from the sender to the receiver. The channel used to communicate a health message influences both what information can be conveyed and how effectively it reaches the audience.
For communication to be effective, the channel must be both accessible and appropriate for the target audience, the channel(s) must be accessible and appropriate for the target audience.
Feedback is the mechanism for assessing what has happened to the receiver after the message is received.
Communication also includes feedback when the receiver responds to the sender. Feedback may be:
A positive effect occurs when the desired change in knowledge, attitude or practice happens. A negative effect occurs when the desired change does not materialize. Either way, feedback provides valuable insight.
This feedback loop allows health communicators to evaluate their effectiveness and adjust their approach to improve future communication outcomes.
Healthcare communication shows up in many forms, each serving a different audience and purpose.
While the content may change, the goal is always the same: to ensure the right information reaches the right people in a way they can understand and use.
Patient-facing materials include all communication designed for patients and their caregivers.
These include:
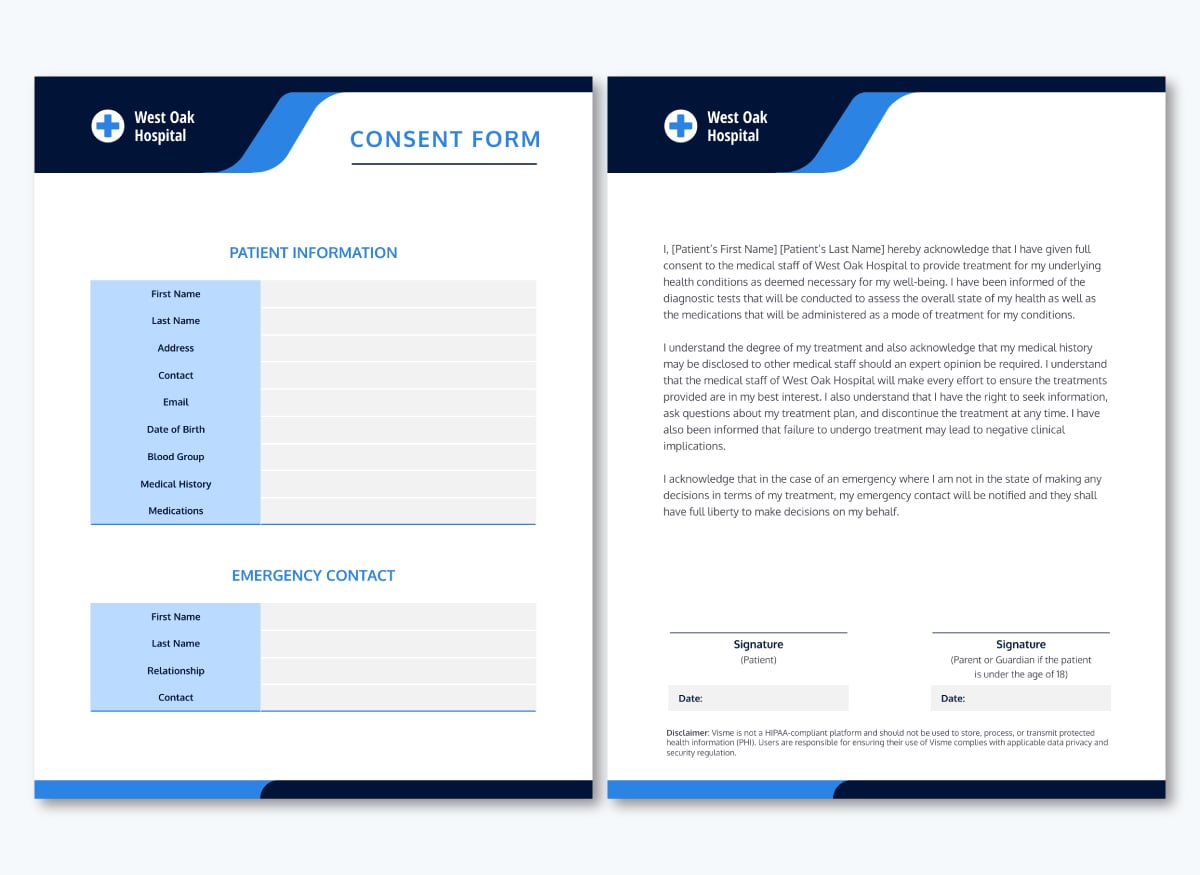
When designing these healthcare and communication materials, it's essential to make them accessible and culturally appropriate so diverse populations can understand and act on the information provided.
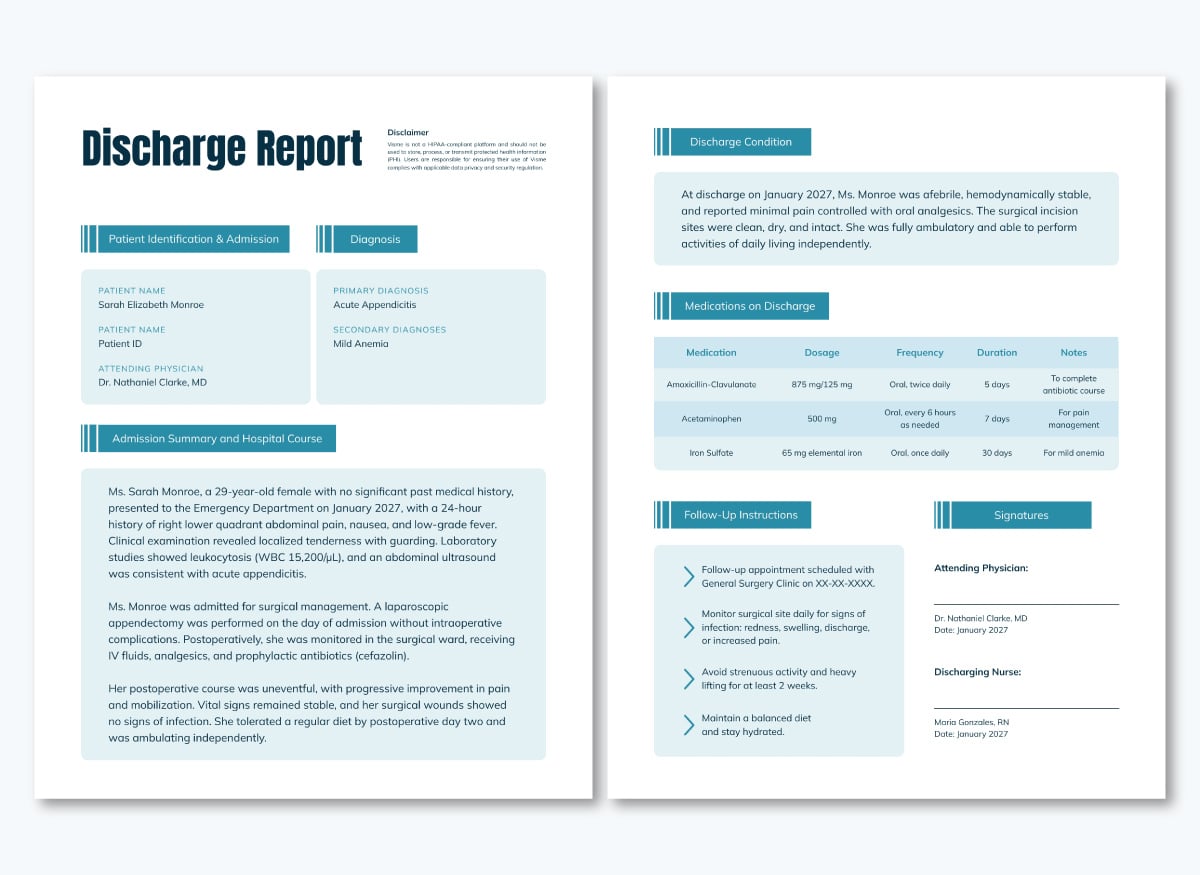
The American Medical Association, the Department of Health and Human Services and the National Institutes of Health recommend that patient-facing instructions be written at a sixth-grade level to ensure adequate comprehension by the average adult. Ensuring discharge instructions are written at the recommended level allows patients to receive information at their health literacy level and improve their overall health and wellbeing.
Here’s why this is important:
Nearly 9 in 10 adults struggle to understand and use health information, especially when it contains complex medical terminology or unclear instructions.
This lack of understanding has severe clinical consequences. Research shows that most hospital discharge instructions are written at levels above recommended readability, making them difficult for patients to follow correctly.
And when patients leave care settings without fully understanding what to do next, health outcomes can deteriorate. Studies have found that many patients do not understand their discharge instructions, especially about medications and follow-up care.
Patient-facing materials can be created in print, digital, visual, interactive and audiovisual formats. These materials are typically shared through various channels:
Internal clinical communication is how care teams stay in sync and keep patients safe. It’s what connects nurses, physicians, pharmacists and specialists as patients move between shifts, departments and locations.
Internal clinical communication covers a wide range of information that supports day-to-day care delivery, including:
When your communication plan template is top-notch, care transitions look coordinated. Everyone knows what’s happening, what’s been done and what needs to happen next.
When it doesn’t, things slip. Details get missed. Orders get misread. Follow-ups get delayed. And those small breakdowns can quickly turn into real problems for patients.
This type of communication is especially tough because it rarely happens in calm conditions. It happens during shift changes, in busy units and under time pressure.
Some of the tools that make it seamless include:


The next important type of communication in the healthcare industry is leadership and operations reporting. It keeps executives, managers and stakeholders informed about organizational performance and strategic progress.
Effective reporting documents performance, surfaces trends, identifies gaps, highlights opportunities and enables leaders to allocate resources strategically.
In multi-site health systems, consistent reporting frameworks ensure that leadership can compare performance across facilities and make system-wide decisions with confidence.
Typically, leadership and operations reports include:
We’ve covered everything you need to enhance training programs in this video below:
These reports are presented at different levels using:
For a long time, healthcare marketing was largely associated with pharmaceutical and medical device companies promoting their branded products. Hospitals, clinics,and care providers didn’t think of themselves as “marketers” until the 1970s. That has changed dramatically.
Today, nearly every part of the healthcare system relies on marketing communication and sales enablement strategies. This includes hospitals, physician practices, managed care organizations, rehabilitation centers, hospices and nonprofits.
The reason is not far-fetched: patients compare providers, employers evaluate health plans and communities expect transparency and accountability. In fact, 63% of consumers will choose one provider over another because of a strong online presence. This stat shows how much branding and communication quality heavily influence trust and decision-making.
Effective marketing communication in sales and marketing materials has become the primary way organizations help audiences understand their:
Here’s a brochure that shares marketing information about a healthcare facility.
Given that these marketing touchpoints span the entire healthcare consumer experience, from learning about a provider to scheduling a visit and receiving care and follow-up care, reliable collaboration between the marketing and technology teams is paramount to achieving seamless healthcare consumer journeys. And to deliver it, an integrated technology stack (across both digital and traditional channels) is essential. - Adam Broitman, Michelle Jimenez and Julie Lowrie, McKinsey & Company.
That integration matters because healthcare marketing rarely lives in a single channel. Instead, it works across multiple touchpoints at once.
In this video, we’ve discussed how to build a healthcare marketing strategy that boosts your visibility, attracts more patients and keeps your practice top of mind.
This type of communication is addressed to everyone within the healthcare organization or system. Unlike patient-facing or marketing communications, systemwide content speaks to internal audiences at all levels, roles and locations. The goal is to create organizational alignment and ensure that everyone, from executives to frontline staff, operates with shared knowledge and understanding.
However, the issue with systemwide communication is achieving both breadth and consistency. In multi-facility health systems, you need to reach diverse audiences simultaneously while maintaining a unified message that accounts for local variations.
A policy update, technology rollout or safety initiative must resonate equally with physicians, nurses, administrative staff and support personnel across different campuses, each with its own workflows and concerns.
Below are the types of communication that fall under this category:

When it comes to distribution, here are channels I’ve found to be effective:
When it comes to communication in healthcare settings, it’s essential to be intentional about how information is created, shared and reinforced across different audiences and settings.
The context might change depending on who you’re talking to, what decision needs to be made, how urgent the situation is and where the communication happens.
But these best practices will help you optimize your healthcare communication strategies.
One of the most common mistakes in communication for healthcare institutions is focusing on the information you have, rather than on what the audience actually needs to understand to move forward.
According to WHO, an effective campaign must also adapt to and consider the context of the community it serves.
The reason isn’t far-fetched. Patients, clinicians, executives and partners all process information differently. So effective communication starts with the question: Who is this for? What do they already know? What decision do they need to make?
An audience-first approach also means recognizing that healthcare serves highly diverse populations.
When working on your healthcare communication design, you ned to acknowledge the diversity of your audience. For patients, consider health literacy levels, language preferences, cultural backgrounds and access to technology.
When dealing with hospital staff, take time pressures, workflow interruptions and information overload clinicians face into consideration. In the same way, leadership and executives are mostly looking at strategic implications, financial impact and actionable insights.
Accessibility should also be an important consideration. Your communication must reach everyone, regardless of language, literacy level, disability status or cultural background.
Vanessa Leonardi, Associate Professor of English Language and Translation at the Italian University of Sapienza, makes an important point about designing truly accessible health content:
'By examining vocabulary, discourse register, syntactic structures and lexical phenomena, researchers can gain insights into how laypersons present and understand information. As a result, the results of such analyses can be used to design and disseminate health information on the internet, highlighting the need for active involvement of medical professionals in ensuring its accuracy and relevance.'
This linguistic perspective reinforces why healthcare professionals must be directly involved in creating patient-facing content, not just reviewing it.
Communicating effectively doesn’t mean you have to dumb things down. It means making information usable.
Research published in Health Affairs shows that low health literacy is associated with higher hospitalization rates and poorer health outcomes, even when access to care is the same. In other words, access alone isn’t enough; understanding is what drives results.
When information is clear and accessible, people are more likely to follow instructions, avoid mistakes and stay engaged in their care or work. When it isn’t, compliance drops and errors increase.
The World Health Organization makes this explicit in its strategic communication framework, which identifies making communication actionable for decision-makers as one of its core principles. The WHO emphasizes that communication should not stop at awareness; it should deliberately move audiences toward action.
This is especially critical in healthcare delivery, where situations can change quickly. During emergencies or rapidly evolving clinical or operational situations, the WHO notes that communicators must adapt their messages to the changing status of the health threat.
It's better to provide accurate guidance quickly and update it as situations evolve than to delay communication while seeking complete information.
Use consistent channels and formats during emergencies so your audience knows where to look for updates. If you establish that critical updates should come via text alert, don't suddenly switch to email-only during a crisis.
The WHO also describes communication as a continuum, not a single event. Effective health communication often follows a step-by-step sequence—building awareness, reinforcing understanding and gradually moving people toward a specific decision or behavior. In other words, good communication anticipates where the audience is now and helps them move to the next step.
Making information actionable starts with being specific and concrete. Avoid jargon whenever possible. If medical or technical terms are necessary, explain them immediately instead of assuming familiarity. For patient-facing materials, aim for a sixth-grade reading level and use readability tools like the Flesch-Kincaid Grade Level or SMOG Index to sanity-check your content.
Actionable communication also means respecting your audience’s time. Long explanations don’t necessarily translate into clarity. Decision-makers, clinicians and patients all need information that gets to the point.
Earlier, I already discussed feedback as a core component of healthcare communication. This is really where good communication gets put to the test.
You can’t assume a message worked just because it was sent. The only way to know is to check. Techniques like teach-back are so effective. Studies have shown that it improves comprehension, medication adherence and patient satisfaction, which is why the Agency for Healthcare Research and Quality (AHRQ) recommends teach-back as a core safety practice.
In patient education, asking patients to explain instructions in their own words gives you a chance to address misunderstandings before they become bigger problems.
The same idea applies beyond patient education. Every communication channel should make it easy for audiences to ask clarifying questions. This might mean Q&A sessions in town halls, comment functions in internal communications or dedicated email addresses for follow-up questions.
When information flows, it’s also important to confirm it’s received and understood. In clinical settings, read-back protocols prevent medication errors. In organizational communication, acknowledgment mechanisms like confirmations, sign-offs or follow-up summaries ensure messages aren’t lost in transit.
Lastly, monitor feedback, complaints, repeated questions and confusion patterns. These signals reveal where your communication is falling short and where you need to adjust.
Effective communication happens through channels your audience actually uses, in formats they prefer, at times when they're receptive.
According to the World Health Organization, communicators must consider a channel’s reach and influence. when developing communications strategies,
“Communicators need reliable channels for reaching decision-makers, disseminating messages and distributing materials. To identify the best available messaging pathways, communicators should analyse the audience’s access to different channels and their preferences.“
In practice, this means adopting a multi-channel approach. Relying on a single method—like email alone—is risky in healthcare environments where inboxes are overloaded and staff are constantly moving.
Important messages are better retained when they’re reinforced across multiple channels. That might include email paired with manager briefings, digital signage on units, short huddles, posted notices or town halls for larger updates.
Channel choice also needs to reflect how people actually work. Many healthcare workers access information on phones or tablets during shifts rather than on desktop computers. If your portals, intranet pages or documents aren’t mobile-friendly, you’re creating friction before the message is even read.
Timing matters just as much as the channel. The WHO also emphasizes that information needs to be shared when people need it, not after the fact.
A well-written update sent at the wrong time can be as ineffective as no communication at all. Sending critical updates late on a Friday afternoon, for example, almost guarantees they’ll be buried by Monday.
Timely communication usually follows a few simple principles: communicate early when possible, share information at moments when people can actually process it and build communication as an ongoing conversation rather than a one-off announcement.
Finally, when you can, respect individual preferences. Patients and staff don’t all want to receive information the same way. Some respond best to text messages, others to email, phone calls or printed materials. Giving people options, especially for non-urgent communication, improves engagement and reduces missed messages.
One of the fastest ways communication breaks down in healthcare is inconsistency.
Different formats, different languages and multiple versions of the same message increase uncertainty and make it harder to trust what information is accurate and up to date.
Standardization reduces that friction. When formats, templates and frameworks are familiar, people know where to find information and what to expect. That matters in high-pressure environments. Studies have found that nurses spend up to 25% of their time searching for information or clarifying orders, often because communication is unclear or scattered across systems.
Here’s how to standardize communication workflows across your healthcare facility:
Healthcare communication happens at scale—across hospitals, clinics, health systems and public health programs. Teams are constantly explaining care, coordinating across roles and guiding people through complex decisions.
In this section, I’ll share examples of healthcare communication that stand out. To make them useful, I’ll also share customizable templates alongside each example, so you can replicate what works instead of starting from scratch.
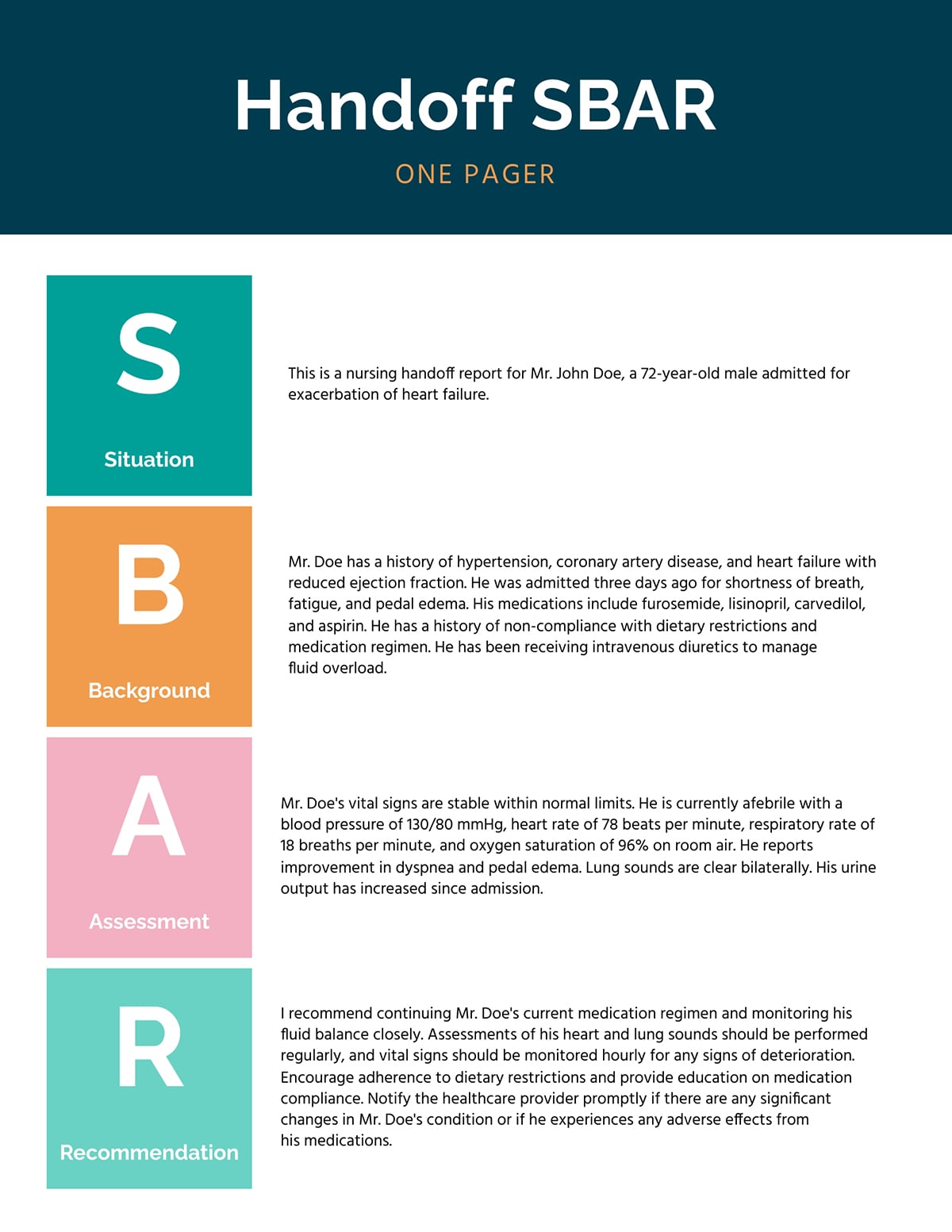
Our first example of healthcare communication in practice is this SBAR implementation and training guide created by the NHS.
The guide tackles one of the most common failure points in healthcare: critical conversations that happen under pressure. It gives teams a simple, shared structure—Situation, Background, Assessment, Recommendation—and then shows them exactly how to use it.
It’s an internal communication material designed for frontline clinical teams and the people responsible for training them. That includes nurses, doctors, allied health professionals, ward managers, clinical educators and improvement leads.
I love how this SBAR guide doesn’t stop at explaining the framework. The content walks teams through what SBAR is, why it matters and how it fits into everyday clinical workflows. It includes real scenarios, training plans, prompt cards, presentations and e-learning resources, so staff aren’t left guessing how to apply it in practice.
Each SBAR component is treated as its own unit. Instead of long explanations, the guide breaks each part into short, scannable sections with clear headings, bullet points and examples. This makes it easy to use in the moment, whether someone is preparing for a handover or training others.
The visuals do a lot of the heavy lifting. Diagrams, callout boxes and prompt cards reinforce the structure so readers don’t have to rely on memory. Most importantly, the guide supports non-linear use. You don’t need to start at page one and work your way through. Someone can dip in, grab a prompt card, review a scenario or scan a checklist and get immediate value.
To replicate this tool in your organization, start by identifying a high-risk communication moment, such as handoffs, escalations, incident reporting or cross-team updates. Then use a one-page SBAR template like the example shown here to standardize how information is shared. Support it with brief training or real examples so teams know how to apply it under pressure.
Our next example is a patient discharge documentation guideline published by the Government of New South Wales. This patient-facing communication tool focuses on one of the most fragile moments in the care journey: the transition from hospital to home or onward care.
Discharge is where communication failures are most likely to show up. Patients are sent home with new medications, follow-up appointments and care instructions—usually while they’re tired, anxious or eager to leave.
The guideline spells out what information must be shared, who is responsible for sharing it and how it should move between hospital teams, patients and primary care providers.
First, the guideline defines required discharge information so critical details aren’t missed or interpreted differently across teams or facilities. This reduces variation, which is a major contributor to post-discharge errors.
Despite being a formal government policy, the content is structured in a way that’s easy to navigate. Distinct sections, definitions and appendices make it easy for staff to quickly find what applies to their roles without having to read the entire document.
I also love how the guideline explicitly states that written discharge summaries alone are not enough. Verbal communication, patient understanding and coordination with primary care are treated as essential parts of the discharge process.
Next in our list of healthcare communication examples is a patient information leaflet from St George’s Healthcare NHS Foundation Trust. This specific example explains what to expect when a child is having an anaesthetic, but it’s part of a much larger library covering procedures, treatments and services across the hospital.
These leaflets are helpful where anxiety, uncertainty and information overload are highest. That’s because parents aren’t just looking for clinical facts; they want reassurance, clarity and a sense of what will actually happen on the day.
This leaflet walks families through the entire experience step by step: before the anaesthetic, during the procedure, pain relief, risks, going home and who to contact if something feels wrong. It also includes links, a QR code for video content and clear contact details so patients and carers aren’t left wondering what to do next.
The language is plain, calm and direct. Medical terms are explained as they appear,
I love how it anticipates questions patients may have. Instead of only explaining the procedure, the leaflet covers practical concerns parents actually worry about: fasting times, comfort items, pain relief at home, emotional reactions after surgery and when to call for help.
Plus, the leaflet doesn’t rely on text alone. It points readers to videos, external trusted resources and support services, recognizing that different people absorb information differently.
It builds trust without overselling. And the risks are explained honestly but proportionately.
Most importantly, it treats patient communication as an ongoing conversation, not a one-time handout. They’ve included contact details, feedback prompts and follow-up resources.
For this next example, we’re looking at a leadership and operations communication piece: an Integrated Performance Report presented to the board by Shrewsbury and Telford Hospital NHS Trust.
This 77-slide board presentation looks overwhelming. But this is the kind of insight healthcare leaders need to see where the organization is doing well, where it’s under pressure and what needs attention. Top management also relies on this type of communication to make decisions that affect staffing, funding, risk and patient care.
Most slides follow a predictable presentation layout: a short summary at the top, visuals in the middle and context or actions on the side. Board members can understand this in seconds, then decide whether they need to dig deeper.
I also love how this board report links performance to action. The results are almost always paired with recovery actions, next steps and timelines. That makes it clear which issues are actively being managed and which need escalation.
The visual cues make decoding information easy for stakeholders. You’ll find tables consistently used to compare performance metrics. And line charts, trend arrows and colour coding are used to show whether performance is improving, holding steady or deteriorating.
If you’re reporting performance for executives or boards using a slide deck, this presentation template is a good starting point. And if leaders need a document format to read at their own pace, we’ve got hundreds of report templates you can easily customize.

Inside the Visme editor, you get access to a full set of data visualization tools in 2D and 3D formats, including line and bar graphs, pie and donut charts, progress indicators, tables, and dashboards. You can connect live data, update visuals in a few clicks and keep layouts consistent across slides and pages.
Before wrapping up this section, it’s worth looking at an example from sales, marketing and broker communication. Email remains one of the most effective channels for reaching healthcare audiences and this Johns Hopkins HealthCare Provider Pulse newsletter shows how structured, well-executed campaigns can drive real engagement and action.
It’s created by Johns Hopkins HealthCare for external clinical partners—physicians, practice managers, billing teams and other providers in its network. Instead of being promotional, it's an operational tool that delivers updates directly affecting provider workflows, reimbursement, referrals and compliance.
The newsletter is built for busy readers. Information is clearly segmented, headings are explicit and nothing is buried in dense blocks of text. Providers can quickly scan the issue, identify what applies to them and move on without feeling overwhelmed.
Each section is concise and action-oriented. The updates focus on what has changed, why it matters and what action—if any—is required. Key details like dates, eligibility criteria and process changes are easy to find, which cuts down on follow-up questions and confusion.
It strikes the right tone as well. The language is professional, neutral and informative, without sounding promotional or overly simplified. I also love how this newsletter follows a predictable structure from issue to issue. Over time, this builds trust and creates a habit—two factors that significantly improve open rates, retention and follow-through. People actually open it because they know what to expect and that it'll be useful.
You can create newsletters like this using Visme's newsletter templates, specifically designed for healthcare organizations. You don’t have to worry about keeping it on brand. Once you input your website URL, our brand wizard pulls in your colors, fonts and logo and saves it in your brand area. That way, you can easily apply it to all communications and ensure brand consistency without manual formatting.
Tap into Visme's library of icons, stock photos and videos and design assets to make your newsletter beautiful and engaging. Add text, section dividers, highlight boxes for critical dates or visual callouts for action items, all without needing a professional design experience.
Once your newsletter is ready, you can distribute it in multiple ways. Send it directly via email, generate a shareable link for your intranet, download it as a PDF for offline access or embed it on your provider portal. Your audience can access it however works best for their workflow.
Here’s a brief overview of popular healthcare communication tools you’ll need for your tech stack. I’ve provided more information about them below the table.
| Tool | Primary Use | Starting Price | Best For | G2 Ratings |
|---|---|---|---|---|
| Visme | Visual content creation & brand management | Free; paid from $12.25/mo | Patient education materials, reports, presentations and infographics | 4.5/5 (450+ reviews) |
| Slack | Internal team communication | Free; paid from $7.25/user/mo | Real-time clinical team coordination, department communication | 4.5/5 (37,000+ reviews) |
| ActiveCampaign | Email marketing & automation | From $15/mo (up to 1,000 contacts) | Patient newsletters, appointment reminders, health campaigns, behavioral automation | 4.5/5 (14,000+ reviews) |
| Descript | Video & audio editing | Free; paid from $16/mo | Educational videos, training content, patient testimonials | 4.6/5 (830+ reviews) |
| Tableau | Data visualization & analytics | From $75/user/mo | Executive dashboards, performance reporting, quality metrics | 4.4/5 (3,450+ reviews) |
| Zendesk | Patient support & helpdesk | From $19/agent/mo | Patient inquiries, appointment scheduling, support tickets | 4.3/5 (6,650+ reviews) |
| TigerConnect | Secure clinical messaging | Contact for pricing | HIPAA-compliant team messaging, care coordination, on-call scheduling | 4.3/5 (6,650+ reviews) |
G2 Reviews: 4.5/5 (450+ reviews)
Visme is the first tool on my list—and for good reason. It’s a true Swiss Army knife for healthcare organizations that need to create professional communication materials without relying on design teams for every request.
Visme gives healthcare teams the flexibility to create a wide range of assets in one place, including patient education materials, clinical and operational reports, executive and board presentations, internal updates, sales enablement content and marketing collateral. When you log in and type healthcare, you’ll find dozens of templates across multiple categories.
I particularly love it for its ease of use. The intuitive, drag-and-drop editor, collaboration tools, millions of design assets and thousands of customizable templates make visual content creation a breeze.
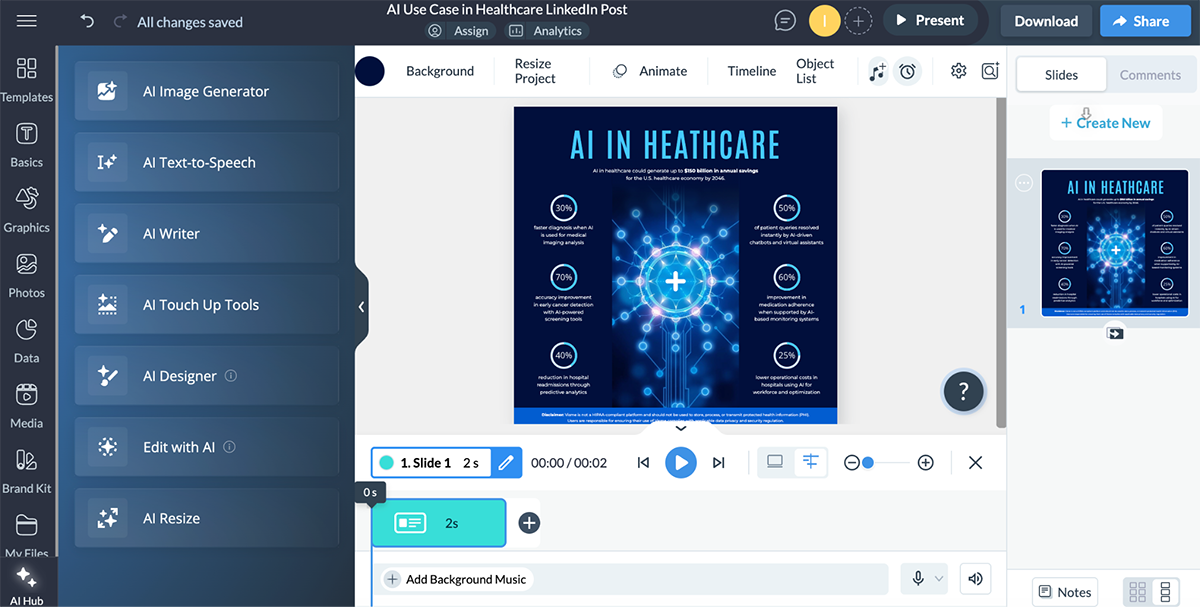
And even if you’re racing against the clock or need a hand with design, Visme has an entire hub of AI tools to speed up your content creation workflow.
G2 Reviews: 4.5/5 (37,000+ reviews)
Slack is a real-time messaging platform designed to cut through the chaos of scattered communication—texts, emails, pagers, hallway conversations—that’s especially common in healthcare environments.
By bringing conversations into one searchable, centralized workspace and connecting with clinical and operational systems, Slack helps teams respond faster and coordinate care more effectively.
What really makes Slack work is how organized and flexible it is. Instead of digging through inboxes or chasing updates, teams have one place where information actually lives. Conversations can happen one-on-one or in channels organized by department, topic or project, so nothing gets lost. You can share files, start quick audio or video huddles when something needs immediate attention and easily search past messages to find that protocol someone shared weeks ago.
It also works well for teams spread across shifts or locations. You can see who’s available, leave messages for others to pick up later and keep work moving without relying on everyone being online at the same time.
G2 Reviews: 4.5/5 (14,000+ reviews)
ActiveCampaign solves a common healthcare communication challenge: how to reach thousands of patients without sending the same generic message to everyone. Instead of one-size-fits-all emails, the platform lets you segment your patient population by age, interests, services used or level of engagement—so people only receive information that's actually relevant to them.
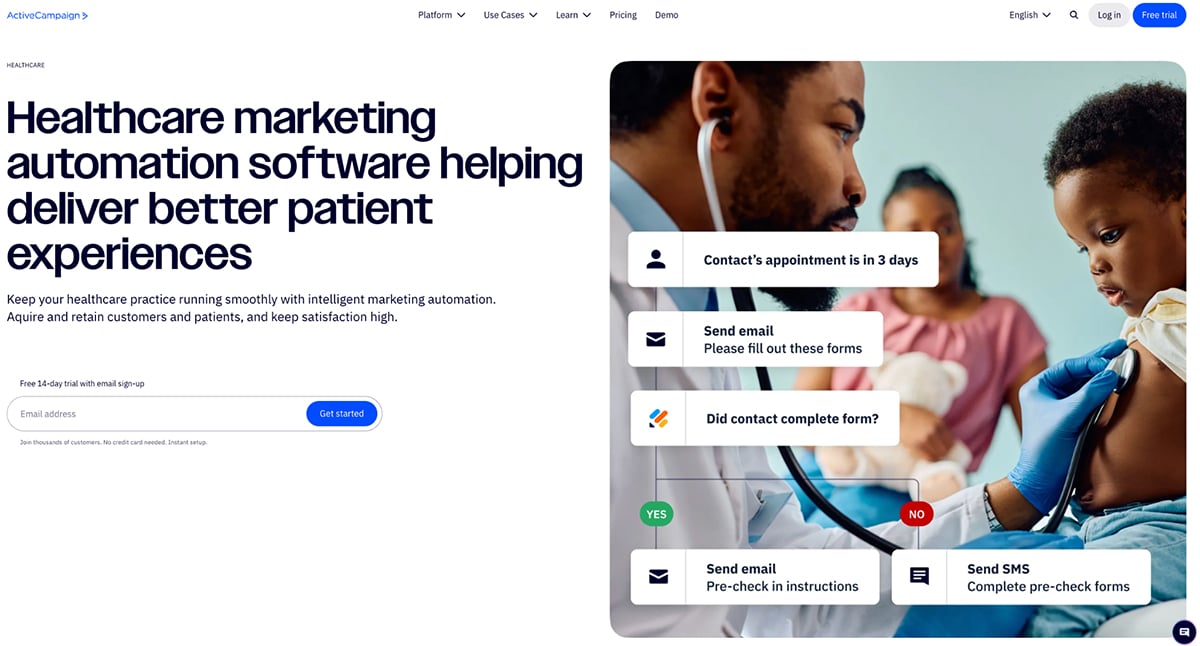
Where ActiveCampaign really shines for healthcare teams is automation. You can set up automated appointment reminders that send themselves, create a welcome series for new patients or deliver targeted health education based on specific needs or behaviors. Once these workflows are built, they run in the background without constant oversight.
ActiveCampaign is also useful for internal healthcare digital communication. Many healthcare organizations use it to send email newsletters to employees, sharing updates, policy changes, training resources and leadership messages in a consistent, professional format.
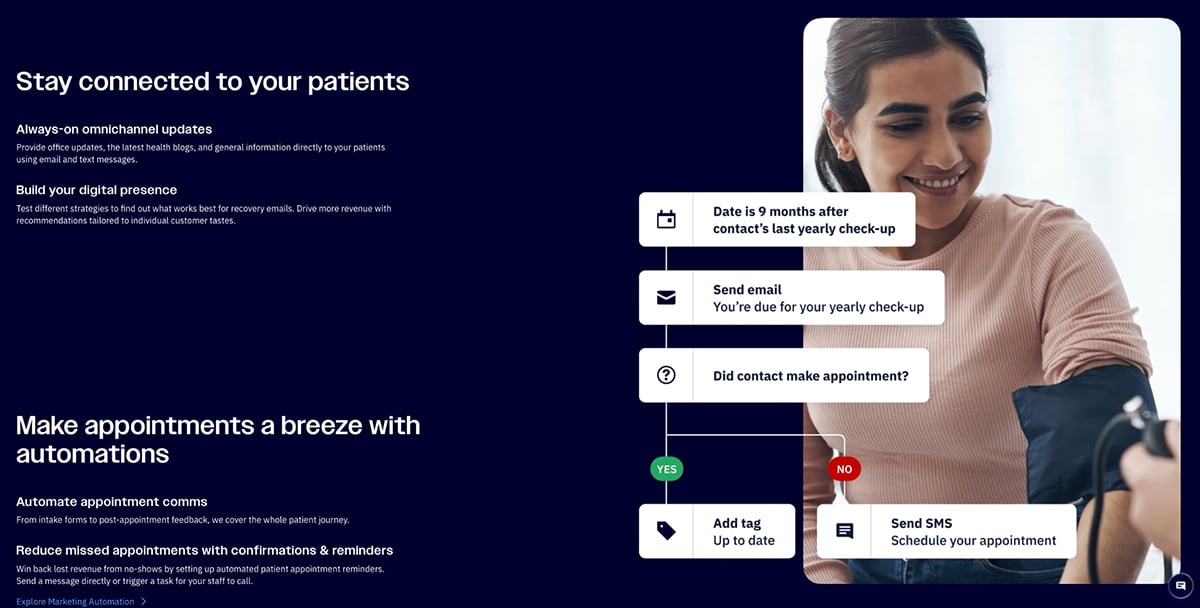
Overall, this takes a huge load off your team. Instead of manually managing contact lists and spreadsheets, staff can focus on strategy and patient experience, while ActiveCampaign quietly handles the execution in the background.
For up to 1,000 contacts
G2 Reviews: 4.6/5 (830+ reviews)
Descript changes how you think about video editing. Instead of wrestling with timelines and complex editing tools, you edit video the same way you’d edit a document—by editing the transcript. Delete a sentence from the text and the corresponding video disappears with it. It’s that straightforward.
I watched a couple of videos and was overly impressed at Descript’s capabilities. For healthcare teams creating training videos, patient education content or procedure walkthroughs, it’s a major time-saver. Clinical experts can record their explanations, then clean up mistakes, pauses and filler words themselves without handing everything off to a video production team.
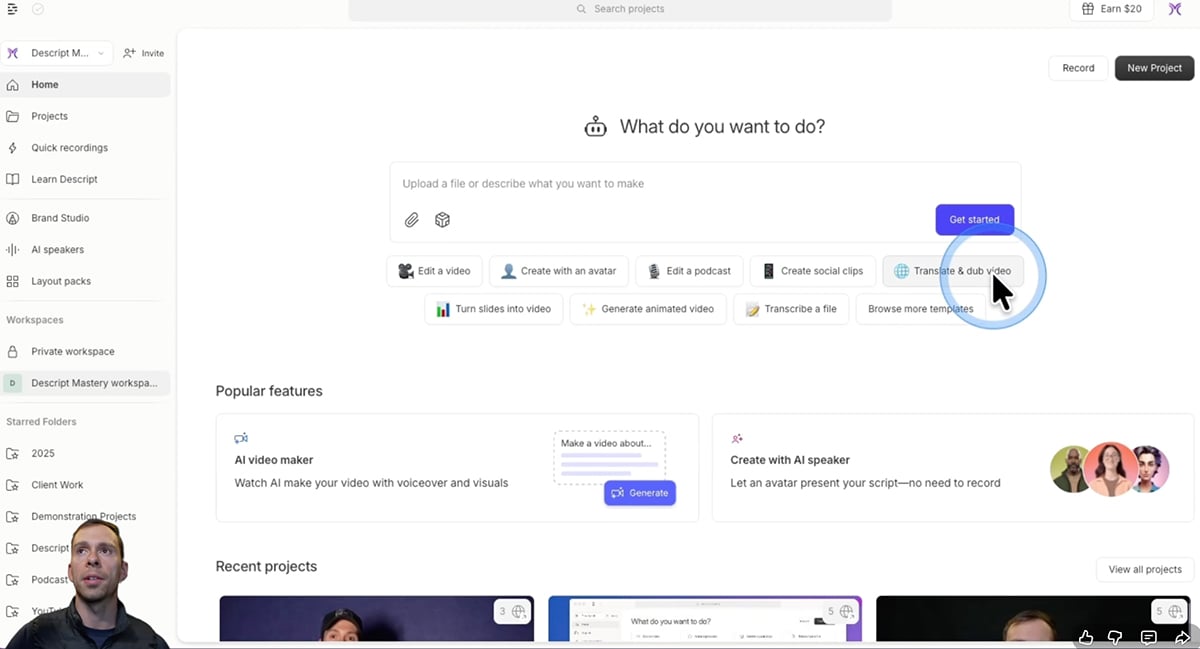
The result is faster turnaround and more control. What used to take weeks of back-and-forth can now be done in hours, making it much easier to keep educational and training content up to date.
G2 Reviews: 4.4/5 (3450+ reviews)
Tableau pulls together scattered healthcare data—from EHRs, financial systems, quality databases and scheduling tools—and turns it into dashboards people can actually use. Instead of waiting on IT to deliver static reports that are outdated by the time they arrive, teams can work with interactive dashboards that update in near real time.
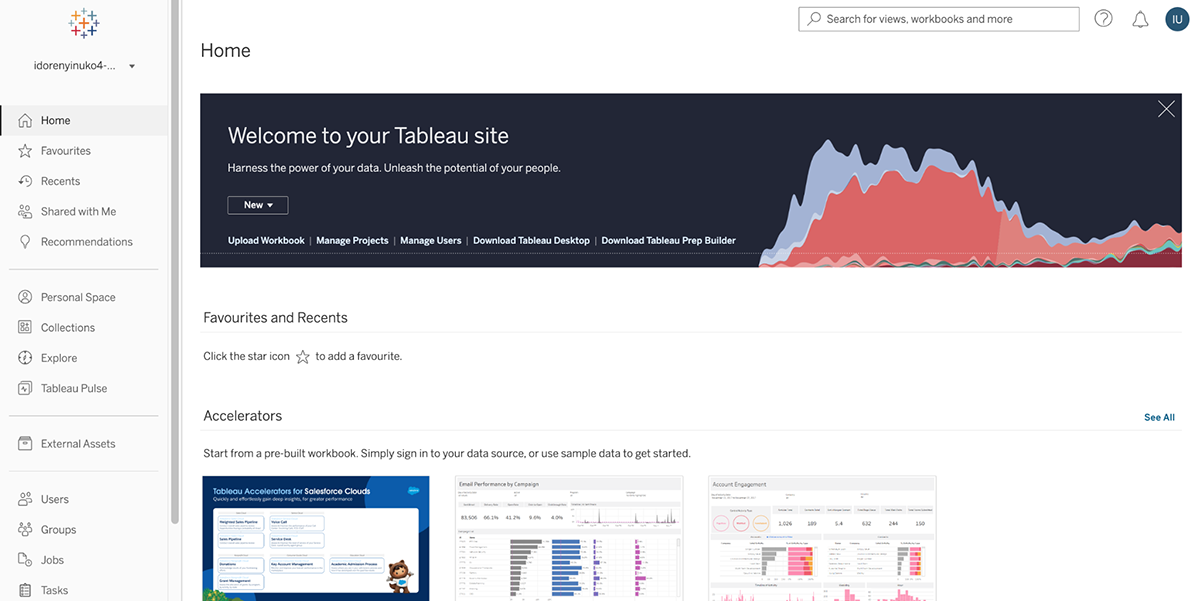
Stakeholders can filter data, drill into details and explore trends on their own, without needing a technical background. That self-service access makes insights easier to find and faster to act on.

For healthcare leaders, the impact is significant. Decisions aren’t based on last month’s numbers or flattened spreadsheets. You’re looking at current data, examining it from multiple angles and spotting patterns and risks that would be easy to miss in basic reports.
https://visme.co/blog/wp-content/uploads/2024/05/10-3.png
G2 Reviews: 4.3/5 (6650+ reviews)
Zendesk is a customer service platform widely used in healthcare for patient support, call center operations, appointment scheduling and inquiry management. It lets you provide omnichannel support across phone, email, chat, text and social media while organizing all interactions (from initial contact through resolution) in a unified ticketing system.
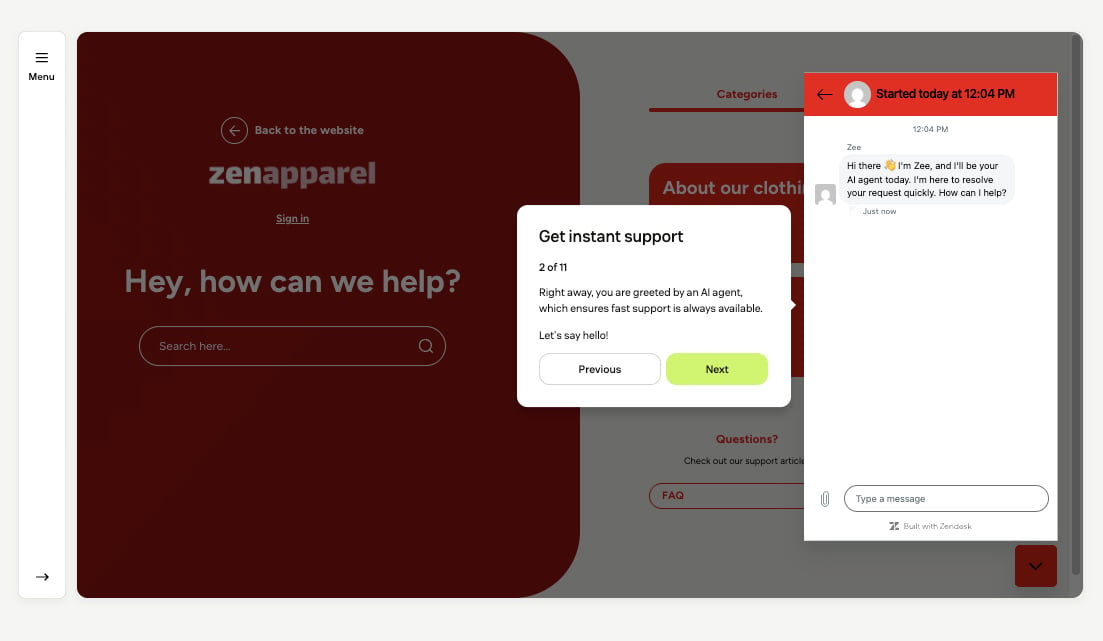
For patient access teams and contact centers, Zendesk solves the challenge of managing high volumes of patient inquiries across multiple channels while maintaining quality, tracking resolution and ensuring nothing falls through the cracks. The platform provides the structure and tools to deliver consistent patient service at scale.
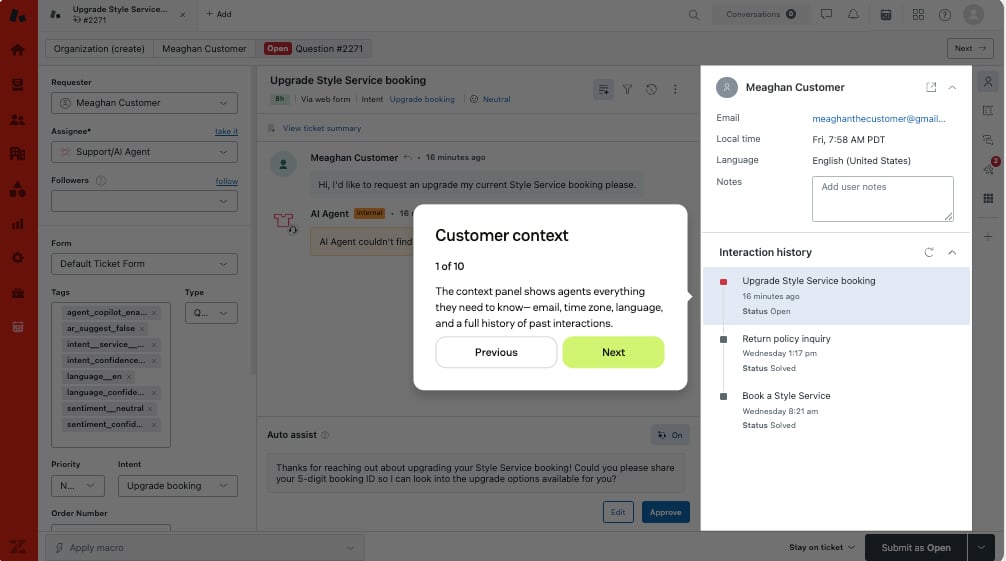
This is important for patient access teams and contact centers that handle hundreds of interactions daily. You need structure. You need to know what's open, what's been resolved, who's working on what and where the bottlenecks are. Zendesk provides the visibility, structure and tools to deliver consistent patient service at scale.
Note: HIPAA compliance available across plans with BAA
G2 Reviews: 4.5/5 (190+ reviews)
TigerConnect is built specifically for secure healthcare communication, which means it gets things that general messaging apps don't. It's HIPAA-compliant right out of the gate, integrates with your clinical systems and includes features designed around how care teams actually work—not how tech companies think they should.
Here's what makes hospital communication tools like TigerConnect different: you can message people by their role instead of hunting down individuals. You can message by role instead of trying to track down specific people ("on-call cardiologist" instead of "Dr. Smith"), integrate with your nurse call system and EHR so alerts come directly to the right person and get delivery confirmation so you know critical messages were received.
The platform handles everything from coordinating patient transfers across facilities to connecting EMS teams with hospital staff before the ambulance even arrives—cutting down time to treatment when minutes matter.
Most communication failures in healthcare stem from a lack of structure.
In a retrospective review of 14,000 in-hospital deaths, communication errors were found to be the leading cause, twice as frequent as errors due to inadequate clinical skill.
Further, about 50% of all adverse events detected in a study of primary care physicians were associated with communication difficulties.
These numbers prove that effective communication in healthcare doesn't happen in isolation. It flows through processes involving multiple people, systems and handoffs.
These communication frameworks and models below act as guiding rails within these processes. They’ll help you map out communication flows end-to-end, identify bottlenecks, standardize best practices and reduce the points where information gets lost.
The 5C Framework gives you five checkpoints to run through before any healthcare communication goes out the door. It works whether you're creating a patient discharge instruction, drafting an internal memo or building a board presentation.
Made with Visme Infographic Maker
Your message should be immediately understandable to your intended audience. No jargon unless absolutely necessary and when you do use technical terms, define them right away. For patient materials, aim for a sixth-grade reading level. For clinical communications, be precise and unambiguous. Vague instructions like "follow up soon" become "schedule a follow-up appointment within two weeks."
Ask yourself: If someone skimmed this in 30 seconds, would they understand the core message and what they need to do?
Respect your audience's time. Every sentence should serve a purpose. This doesn't mean leaving out important information;it means cutting everything that doesn't add value.
Healthcare professionals are drowning in information. Patients are overwhelmed and anxious. Neither group benefits from unnecessary words. Get to the point, organize information logically and use formatting to make key points scannable.
Accuracy is a non- negotiable in healthcare. Wrong medication dosages, incorrect contact information or outdated protocols can cause serious harm.
Build verification into your process. Have clinical subject matter experts review patient materials. Double-check data before including it in reports. Establish review cycles to keep content current as medical knowledge and organizational policies evolve.
Healthcare communication happens in stressful contexts. People are worried about their health, grieving losses, making difficult decisions or working under intense pressure.
Tone matters. Even in clinical or operational communications, you can be both professional and human. Acknowledge uncertainty when it exists. Show empathy for the situation your audience is facing. Avoid language that blames or shames.
For patient communications specifically, anticipate fears and questions. Don't just tell someone what to do, explain why it’s super important.
Below are popular communication models used in the healthcare industry.
Made with Visme
SBAR is probably the most widely adopted healthcare communication workflow, originally developed by the U.S. Navy and adapted for healthcare. It structures urgent or critical communications between clinicians.
SBAR reduces miscommunication by ensuring critical information follows a predictable pattern. The receiving provider knows what to listen for and the calling provider doesn't forget crucial details under pressure.
You can use it for clinical handoffs, urgent consultations, nurse-to-physician communication, rapid response situations, any time you need to escalate a patient concern quickly
Made with Visme Infographic Maker
I-PASS is designed specifically for patient handoffs between shifts or between care teams. Research shows I-PASS delivers measurable results. Here’s how it works:
The read-back component is what makes I-PASS particularly effective. it catches misunderstandings before the handing-off provider leaves. The contingency planning also prepares the receiving team for likely complications instead of leaving them to figure it out from scratch at 2 AM.
You can use it during shift changes, transfers between units (ED to floor, floor to ICU), handoffs from outpatient to inpatient teams and rotation changes for residents and fellows.
Made with Visme Presentation Maker
The REDE MODEL focuses on building and maintaining therapeutic relationships with patients across three phases. It applies effective communication skills to optimize personal connections in three primary phases of Relationship: Establishment, Development and Engagement (REDE).
REDE recognizes that healthcare relationships aren't transactional; they're ongoing partnerships that has to be intentionally cultivated.
Relationship engagement alone has been found to enhance health outcomes by improving patient comprehension and recall, capacity to give informed consent, patient self-efficacy, treatment adherence and self-management of chronic illness.
This model is useful in primary care relationships, chronic disease management and oncology care.
Made with Visme Infographic Maker
CICARE was developed to standardize patient interactions and ensure every encounter feels personalized and complete. It's particularly popular in hospitals focused on patient experience.
Here’s how it works:
CICARE creates consistency across your organization. Whether patients interact with physicians, nurses, transporters or environmental services, every encounter follows a recognizable structure that feels respectful and complete. This consistency builds trust and reduces anxiety.
It’s useful for every single patient interaction, including bedside rounds, medication administration, procedures, discharge planning, even brief check-ins.
Developed by Kaiser Permanente, the Four Habits Model structures entire clinical encounters around four key practices that improve patient-provider relationships and outcomes. They include:
The Four Habits improve both patient satisfaction and clinical outcomes because they ensure patients feel heard, understood and partnered with—which increases adherence and trust. The model is comprehensive enough to guide entire visits while being practical enough to remember and use consistently.
Made with Visme Presentation Maker
LEARN is specifically designed for navigating cultural differences and health literacy gaps. It's built on the recognition that effective healthcare requires cultural humility and the ability to bridge different worldviews.
LEARN explicitly addresses the reality that patients come from diverse backgrounds with different health beliefs, literacy levels and cultural practices. By negotiating rather than dictating, you create plans patients will actually follow—which matters more than the theoretically perfect plan they'll abandon.
Use it when interacting with patients from different cultural backgrounds, situations where health literacy is a barrier, any time you sense resistance or non-adherence rooted in differing beliefs or values or chronic disease management requiring lifestyle changes.
SEGUE is a research-based tool widely used in medical education to teach and assess doctor-patient communication. t stands for
SEGUE provides a comprehensive checklist that ensures you don't miss critical communication elements. You can deploy for clinical encounters in any setting, particularly useful for training medical students and residents and quality improvement efforts.
So what’s the best framework institutions should adopt?
There’s no one-size-fits-all model. The right model depends on what you're trying to accomplish. Some are built for urgent clinical situations, others for building patient relationships and still others for navigating cultural differences.
AI is changing how healthcare organizations create, manage and deliver communication.
But the conversation around AI in healthcare often focuses on clinical applications—diagnosis support, drug discovery and radiology interpretation.
What gets less attention is how AI is transforming the communication infrastructure that holds these organizations together.
The opportunity here is significant, but so are the risks. Use AI thoughtfully and you can dramatically improve efficiency, personalization and accuracy. Use it carelessly and you introduce new sources of error, bias and compliance violations.
Here’s how to use AI within your communication workflow.
Healthcare organizations need to produce massive volumes of visual communication materials. This includes patient education handouts, interactive clinical presentations, infographics explaining procedures, discharge instructions, health campaign graphics and staff training materials.
Creating these typically requires either graphic design expertise or lengthy back-and-forth with design teams. This situation creates bottlenecks that delay important marketing, clinical and leadership communications.
AI-powered design platforms like Visme’s AI Designer generate professional healthcare visuals in minutes. These solutions empower clinical teams, patient educators and communication staff to create materials themselves without design skills or waiting for creative departments.
Healthcare serves diverse populations with varying needs. This includes patients who speak different languages, those with visual impairments or reading difficulties, individuals with low literacy and people who simply prefer audio content.
Creating audio versions of patient materials traditionally requires professional voiceover services, expensive recording equipment and significant time. Translating materials into multiple languages adds even more complexity and cost. That explains why you see English-only materials by default, which leaves non-English speakers at a disadvantage.
AI text-to-speech tools, such as Google Cloud Translation, Visme’s AI text-to-speech tool, DeepL, etc. converts written materials into natural-sounding audio in multiple languages instantly. These healthcare communication solutions make information accessible to broader populations without the cost and delay of traditional voiceover production.
A huge portion of healthcare communication exists just to keep people on track: appointments, test results, follow-ups, referrals, and medication checks. When these messages are lost in transit, medical care process breaks down.
AI is increasingly used as the connective tissue between these steps.
Instead of relying on manual calls and static reminders, AI systems can now confirm appointments, handle rescheduling, send follow-up instructions and flag patients who are likely to miss care based on past behavior.
Or instead of staff manually copying information from one tool to another, AI can:
Platforms like Twilio Health, Relatient and TeleVox already use AI to automate appointment flows and follow-up communication across SMS, voice and email.
Healthcare professionals are overwhelmed by messages from patients, from colleagues, from systems. AI isn’t here to replace clinical conversations, but it can support them in real time.
Some tools are now trained on peer-reviewed medical content and clinical guidelines so they can surface evidence-based information when it’s needed.
For example, Skyscape’s Buzz Lightning provides contextual clinical answers and decision support inside a HIPAA-compliant environment. Instead of searching across multiple systems, clinicians can ask one question and receive relevant, trusted information instantly.
This doesn’t make decisions for providers. It helps them communicate and act with more confidence, especially under time pressure.
Writing patient messages, updating records, responding to portal questions and documenting care takes enormous mental energy. Even when the task is small, the constant switching drains clinicians.
Generative AI is now being used as a co-pilot, not a replacement. Tools like Microsoft Dragon Copilot, Nuance DAX and Laguna Insight help summarize conversations, draft follow-up notes and prepare responses that clinicians can review and personalize.
One of the clearest real-world examples comes from UC San Diego Health, one of the first systems to pilot generative AI for drafting replies to patient messages inside Epic.
“We are very interested in using AI to help solve health system challenges, including the increase in patient messages that are contributing to physician burnout,” said Christopher Longhurst, MD, chief medical officer and chief digital officer at UC San Diego Health. “The evidence that the messages are longer suggests that they are higher quality and the data is clear that physicians appreciated the help, which lowered cognitive burden.”
The study found that although AI did not reduce response time, it significantly eased the mental effort of writing.
“Our physicians receive about 200 messages a week. AI could help break ‘writer’s block’ by providing physicians an empathy-infused draft upon which to craft thoughtful responses to patients,” said Ming Tai-Seale, PhD, lead author of the study.
Even after long shifts, clinicians said AI helped them respond more thoughtfully.
“AI doesn’t get tired, so even at the end of a long day, it still has the capacity to help draft an empathetic message while synthesizing the request and relevant data into the response,” said Marlene Millen, MD, chief medical information officer for ambulatory care at UC San Diego Health.
Ultimately, this study from the University of California, San Diego found that AI-assisted communication significantly reduced the mental effort required to write personalized messages — even when it didn’t change response time. The impact was emotional and cognitive, not just operational.
That matters in a system where burnout is driven as much by invisible work as clinical demand.
You promote effective communication by creating structure, not just sharing information. That means using clear frameworks for handoffs, standard templates for reports and patient materials and feedback loops to confirm understanding.
It also means training teams on how to communicate under pressure, using tools that reduce manual work and making information easy to access across departments and systems. When communication is consistent, timely and audience-focused, it becomes part of the care process—not a separate task.
The four most common types are:
Common techniques include active listening, teach-back, plain language, structured handoffs (like SBAR), visual aids and two-way feedback. These healthcare communication techniques focus on clarity, empathy and confirmation so information is not only delivered, but understood and acted on.
The 7 C’s are a simple way to check whether your message is effective:
Healthcare communication must meet all seven to be safe and useful.
Written communication includes anything documented or shared in text form, such as clinical notes, discharge summaries, patient letters, policies, reports, emails and patient portal messages. Because written information is often referenced later, it must be accurate, accessible and easy to understand.
Start by using plain language, checking for understanding with teach-back and giving patients clear next steps. Offer information in multiple formats—written, visual and audio—so people can choose what works for them. Most importantly, make communication a conversation, not a one-way message.
Common barriers include medical jargon, language differences, low health literacy, time pressure, emotional stress, cultural differences, fragmented systems and lack of standard processes. These barriers don’t disappear on their own—healthcare leaders must actively design around them with proven frameworks, accessible formats, and supportive technology.
Healthcare communication has never been more complex or more critical. You're managing patient education across diverse populations, coordinating clinical teams in real-time, keeping leadership informed with meaningful data, engaging communities through multiple channels and doing it all while meeting strict compliance standards.
This guide has shown how communication touches every corner of healthcare: clinical safety, operational efficiency, patient trust and organizational performance. But knowing what to do is only part of the equation. You also need tools that help your teams act quickly without sacrificing quality, brand consistency or compliance.
Visme gives healthcare teams a simple way to turn complex information into clear, visual communication, whether you’re creating patient education materials, leadership reports, training resources or marketing content. With customizable templates, interactive charts, AI-powered design tools, brand controls, approval workflows and secure sharing, Visme helps you create compliant, on-brand communication at scale.
If you’re ready to simplify how your organization communicates and create materials people actually understand and use, explore how Visme supports healthcare teams here.
Design visual brand experiences for your business whether you are a seasoned designer or a total novice.
Try Visme for free